Over the past few years, there has been a lot of news surrounding the availability of Adrenaline Auto-Injectors (AAIs) such as Epipen. My favourite story is the almost comic villainisation of Heather Bresch from Mylan in the US who, seeing an opportunity in the market increased the price of Epipen by 461% and as a consequence received a 671% pay raise.
The latest bit of news which has hit the Pharmacy Popular Press in the UK, direct from the DHSC Supply Disruption Alert, is that pharmacists must implement controls of the child dose of adrenaline 150mcg AAIs. To streamline this restriction, the DHSC has created this simple flowchart:

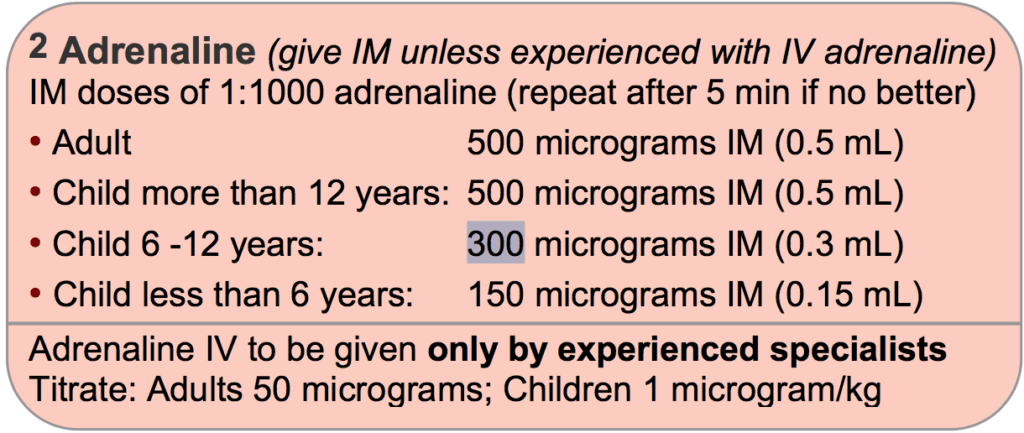
Essentially, it is a triage for supply to the most in need. i.e. if the patient is over 25kg they need to go to the prescriber who should change the patient to the 6-12-year-old 300mcg dose. This is contrary to what is considered best practice recommended by the Resuscitation Council Guidance 2015.
Obviously, before releasing the DHSC the NHS has considered this and consulted the Council for their blessing. However, I would be surprised if they explored all of the potential options for addressing this problem.
There are three potential formulations when it comes to Adrenaline administration. An auto‐injector is considered the choice formulation as it allows early administration of adrenaline in comparison to other formulations, as this has been shown to improve outcome. It is often seen as a quick simple to use first‐aid measure combined with calling for help (ambulance/emergency medical services). In medicine, this would be considered a “first line treatment” i.e. the best formulation for that patient at that specific time. Whereas in a hospital you are more likely to see the other formulations i.e. Ampoules and needle or a pre-filled syringe. These formulations are often reserved for those who have had a little more training about how to administer them as it can be somewhat time-consuming to prepare which is important as there is a strong correlation between detrimental effects of anaphylaxis and time taken to administer adrenaline. However, it is well known in General Practice about the over-prescribing of AAIs.
To the point. Why does the NHS instead of going against best practice, not make a scheme where the pharmacist can train willing patients about how to use other formulations? The answer to this is complex but I think one reason is the lack of knowledge of pharmacist skill set. Ever since the release of the national pharmacy flu PGD in 2016 every pharmacist in the UK has a contractual duty to offer flu vaccines. Every person administering a flu vaccine must be well versed in Anaphylaxis protocols. Why dont pharmacists use this opportunity to perform an intervention MUR on the patient and try to figure out if other formulations might be appropriate? This would not only save money, but it would also make the patient more proficient in administering the correct best practice dose.
